One of the most controversial topics in the healthcare world is the debate over when and how to move to a fully interoperable health data ecosystem. In an ideal world, a collection of coordinated, universal, un-hackable systems would securely host the health data of every person in the country (or world). This data would be accessible across clinical, laboratory, medical, pharmaceutical, and personal uses, regardless of location, applications, or vendors. But, that’s the ideal situation. At present, we’re far from true healthcare interoperability. In the first post of our 3-part series, we’ll examine what healthcare interoperability is, the three levels of interoperability, and EnsoData’s vision for the interoperability requirements needed to usher forward the future of sleep medicine and patient care.
 As the infographic mentions, a system that integrates at all three levels of i14y is the holy grail of interoperability, and some companies, like us, are making this semantic level the focus of their development, knowing it is the future of healthcare.
As the infographic mentions, a system that integrates at all three levels of i14y is the holy grail of interoperability, and some companies, like us, are making this semantic level the focus of their development, knowing it is the future of healthcare.
What is Healthcare Interoperability?
Interoperability, often abbreviated as i14y in the tech community, refers to a computer system’s ability to communicate and exchange fundamental data elements with other systems. A fully interoperable system is one whose interface, data, and products are completely understandable to outside systems, and vice versa. Not only that, but access must be past, present- and future-facing, with adherence to data standards, clinical ontologies, and best practices. A 2008 congressional act, the 21st Century Cures Act, (Cures Act), put meaningful use and care quality measures behind interoperability in the healthcare space by demanding through public policy that healthcare organizations big and small achieve the following i14y ends:- Enable the secure exchange and use of electronic health record (EHR) data information without special effort or technology on the part of the user
- Allow for complete access, exchange, and use of all electronically accessible EHR data for authorized use under applicable law
- Do not participate in “information blocking”
What are the three levels of Healthcare Interoperability?
The three levels of healthcare interoperability are the foundational level, the structural level, and the semantic level. Each of the three levels dives into the interoperability discussion with a different lens, and builds upon the previous stage.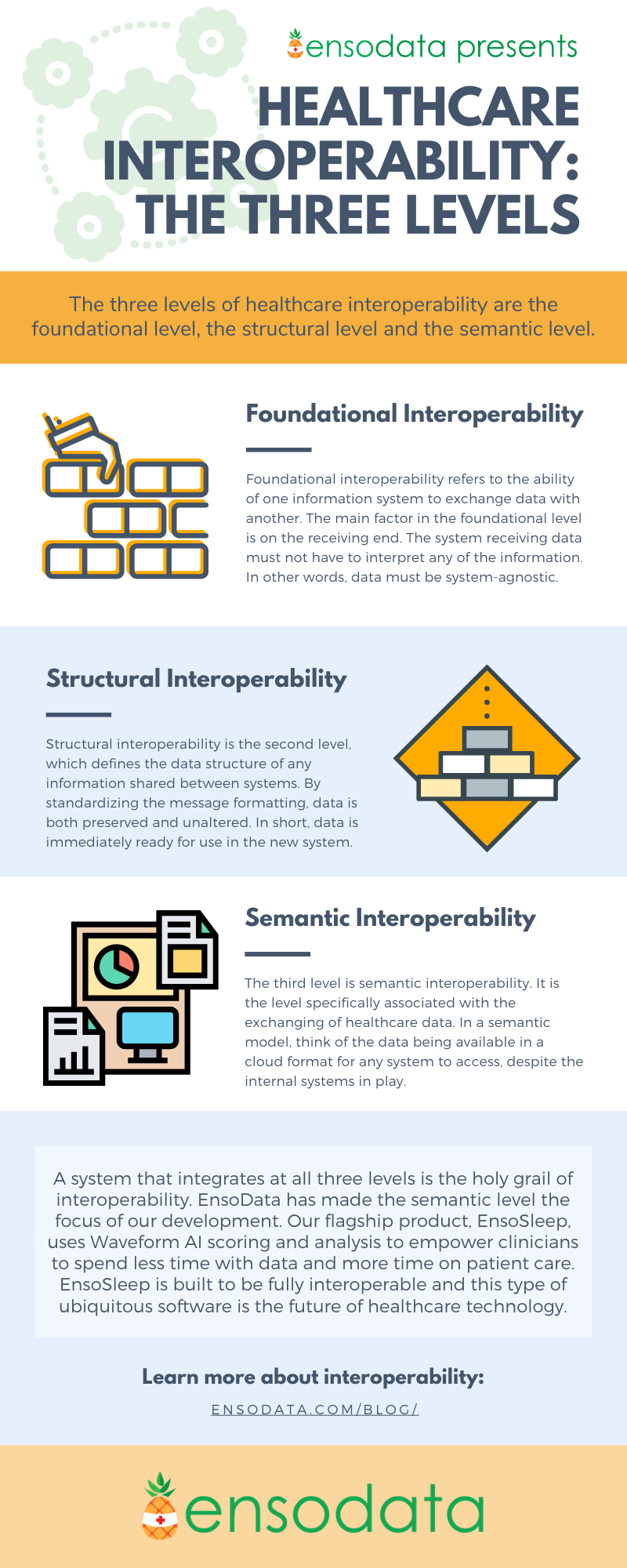 As the infographic mentions, a system that integrates at all three levels of i14y is the holy grail of interoperability, and some companies, like us, are making this semantic level the focus of their development, knowing it is the future of healthcare.
As the infographic mentions, a system that integrates at all three levels of i14y is the holy grail of interoperability, and some companies, like us, are making this semantic level the focus of their development, knowing it is the future of healthcare.