Conducting a COVID-19 Sleep Center Impact Study
To collect the data discussed in our downloadable COVID-19 Sleep Center Impact Study, we conducted 100 phone interviews of leading sleep medicine clinicians and operators at sleep clinics. This list included a range of Sleep Center executives, operations managers, physicians, technologists, and related allied health professionals. We asked this group a series of structured questions to generate data points and we discussed their situations anecdotally. In conducting this research, we hope to equip sleep medicine professionals with practical information to consider at their organizations. From restoring access, to scaling new or existing home sleep testing (HST) volumes and Telehealth capabilities, we urge sleep centers to invest in their future.COVID-19’s Impact on Sleep Centers
 This pandemic has been especially hard on In-Lab Sleep Centers, with major reductions in diagnostic, split-night, and titration PSG studies.
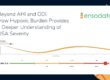
As part of the EnsoData sleep center impact study, 72% of participants reported a temporary suspension of all in-lab sleep testing operations. The majority of these suspended operations are located in urban and suburban areas, and consistently had stricter at-home mandates than their rural counterparts.
Additionally, of the 28% of respondents that have not suspended study operations, most are concentrated in lower density and lower population areas, including centers from rural regions of Mississippi, Wyoming and South Dakota.
In other words, for In-Lab testing, just under 3 in 4 sleep centers have had to suspend their operations. That’s a huge chunk of our testing community, and yet, there was a glimmer of light on the home sleep testing front.
This pandemic has been especially hard on In-Lab Sleep Centers, with major reductions in diagnostic, split-night, and titration PSG studies.
As part of the EnsoData sleep center impact study, 72% of participants reported a temporary suspension of all in-lab sleep testing operations. The majority of these suspended operations are located in urban and suburban areas, and consistently had stricter at-home mandates than their rural counterparts.
Additionally, of the 28% of respondents that have not suspended study operations, most are concentrated in lower density and lower population areas, including centers from rural regions of Mississippi, Wyoming and South Dakota.
In other words, for In-Lab testing, just under 3 in 4 sleep centers have had to suspend their operations. That’s a huge chunk of our testing community, and yet, there was a glimmer of light on the home sleep testing front.
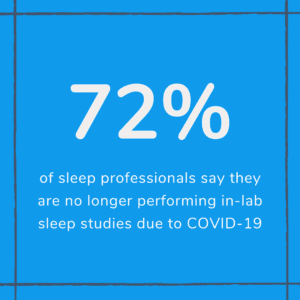
 When asked about HSTs, 79% of sleep centers confirmed that they’ve maintained the same level of patient access as they were seeing pre-COVID-19.
Anecdotally, respondents credited an increased adoption of direct-ship home testing models. The alternative methods that adhere to social distancing guidelines have thrived, which has even resulted in unexpected net new gains for some sleep centers.
At-home diagnostic remote care solutions – like direct-ship HSTs and Telehealth administrative services – have been the biggest winner in the sleep testing world.
These technologies enabled some sleep centers to expand home testing programs without spending additional capital on devices and inventory or investing time in IT to spin up and maintain video appointment software.
In the current climate, pairing video and phone evaluations (on the front line) with HSTs (on the back end) has been a necessity, but it may ultimately become the norm.
According to our respondents, of the supermajority of Sleep Centers conducting home sleep testing, 48.4% reported an active increase in HST volumes requiring investment in new and/or additional HST infrastructure [3]. That’s right, growth. Not delays, not suspensions, but new revenue. And our anecdotal commentary backs that data up:
When asked about HSTs, 79% of sleep centers confirmed that they’ve maintained the same level of patient access as they were seeing pre-COVID-19.
Anecdotally, respondents credited an increased adoption of direct-ship home testing models. The alternative methods that adhere to social distancing guidelines have thrived, which has even resulted in unexpected net new gains for some sleep centers.
At-home diagnostic remote care solutions – like direct-ship HSTs and Telehealth administrative services – have been the biggest winner in the sleep testing world.
These technologies enabled some sleep centers to expand home testing programs without spending additional capital on devices and inventory or investing time in IT to spin up and maintain video appointment software.
In the current climate, pairing video and phone evaluations (on the front line) with HSTs (on the back end) has been a necessity, but it may ultimately become the norm.
According to our respondents, of the supermajority of Sleep Centers conducting home sleep testing, 48.4% reported an active increase in HST volumes requiring investment in new and/or additional HST infrastructure [3]. That’s right, growth. Not delays, not suspensions, but new revenue. And our anecdotal commentary backs that data up:
“We started moving to virtual HST and CPAP set-ups back in September, with 50 per month then,” said the COO of an East Coast Sleep Center. “Currently, we’re doing around 290 virtual CPAP setups per month.”The new customer demand is for quality, convenience and personal safety. With this demand, the turn-key value in the new HST model has it positioned to become the new norm.
Telehealth and Telemedicine are Booming
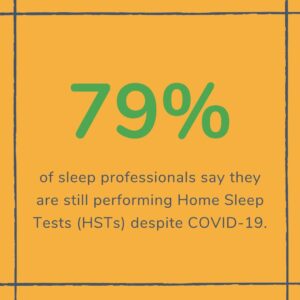
Of our interviewees, 64% of sleep centers said they were actively using Telehealth and telemedicine technology platforms. While video and phone based appointments and consultations are the biggest use cases, respondents highlighted a handful of beneficial applications:- Performing virtual diagnostic evaluations
- Discussing confidential treatment alignment and prescriptions with patients
- Executing the clinical management of CPAP adherence
- Providing proactive follow-up, outreach, and education about CPAP equipment cleaning best-practices
- Educating staff and patients on updated COVID-19 information for high-risk patients
 The uses of technology are always endless, but in a time of crisis, technology uses grow from necessity rather than from simple choice. For the 36% of Sleep Centers that have yet to start offering Telehealth based appointments, there were a number of factors including reduced budgets and unexpected staffing changes. Many pulmonary staff members have been shifted to acute care to support the fight against the coronavirus, and other medical areas have been impacted.
In a post-COVID-19 world, the forward-thinking sleep centers may choose to focus on the sustainable changes we’ve seen to the ratio of at-home testing compared to in-clinic care. Pre-COVID-19, this was a 70/30 split, but in the long term, a pivot may be made to more HSTs simply due to cost simplifications and center efficiencies that have been discovered during the crisis.
For example, staffing challenges related to uncontrollable conditions (like this pandemic) may happen again and without warning. The effects on patient care demand and on consumer price sensitivity go beyond the control of our industry, as well, bowing to national changes in employment. To proactively prepare for the future, it can be in the best interest of a sleep center to shift to a more tech-focused solution.
Sleep Center enterprise tools and technologies aimed at increasing the efficiency of clinical operations, capacity, and home-based care will always be top priorities for sleep medicine practitioners. Never before has that been so obvious as during this shift in operations caused by the coronavirus.
The numbers speak for themselves: HSTs were far more productive during this pandemic when compared to their in-office counterparts. Businesses of all kinds must adapt, iterate, and evolve to succeed.
The uses of technology are always endless, but in a time of crisis, technology uses grow from necessity rather than from simple choice. For the 36% of Sleep Centers that have yet to start offering Telehealth based appointments, there were a number of factors including reduced budgets and unexpected staffing changes. Many pulmonary staff members have been shifted to acute care to support the fight against the coronavirus, and other medical areas have been impacted.
In a post-COVID-19 world, the forward-thinking sleep centers may choose to focus on the sustainable changes we’ve seen to the ratio of at-home testing compared to in-clinic care. Pre-COVID-19, this was a 70/30 split, but in the long term, a pivot may be made to more HSTs simply due to cost simplifications and center efficiencies that have been discovered during the crisis.
For example, staffing challenges related to uncontrollable conditions (like this pandemic) may happen again and without warning. The effects on patient care demand and on consumer price sensitivity go beyond the control of our industry, as well, bowing to national changes in employment. To proactively prepare for the future, it can be in the best interest of a sleep center to shift to a more tech-focused solution.
Sleep Center enterprise tools and technologies aimed at increasing the efficiency of clinical operations, capacity, and home-based care will always be top priorities for sleep medicine practitioners. Never before has that been so obvious as during this shift in operations caused by the coronavirus.
The numbers speak for themselves: HSTs were far more productive during this pandemic when compared to their in-office counterparts. Businesses of all kinds must adapt, iterate, and evolve to succeed.
Your Formula for Success
The challenges of this crises are infinite, with each day spinning up something different than the day before. For organizations, there are structural, financial and logistical obstacles. For clinicians, day-to-day life has shifted dramatically, especially for those who have been redirected to the front line of the battle with this virus. And, for sleep leaders at organizations, the challenges start with figuring out how to get more work done with half the resources. The backlog of in-lab sleep studies (which in many cases was already a 3-4 month wait) has been growing steadily for most organizations. With a lack of staff to execute and score sleep tests, leaders have been forced to make difficult decisions and changes, specifically in regards to testing logistics, scoring, and cleaning and maintenance. For clinicians, the experiences obviously have a drastic range of outcomes. For some, this has been a true test of resilience and bravery. In our interviews, we did hear that clinicians have been shifted to the frontline of critical care, some with inadequate safety supplies and ventilatory support machinery. Those lucky to remain in sleep centers have been asked to handle larger patient loads. And, unfortunately, still others have been added to the nation’s unemployed or furloughed lists. In-Lab focused operations in urban areas were particularly impacted, but sleep centers around the country have been confronted with the dilemma: get with the technological times or fall behind. And while it’s not COVID-19 focused, several clinician participants in the study advised others participating to remember to get their own good sleep, as well. Practice what you preach.Newly Discovered Sleep Testing Best Practices
The best practices themselves were imprinted clearly in the data collected, and we say as much in the downloadable report. But to provide a TL/DR version of the above, here are the key bullet points:- Sleep centers that relied exclusively on In-Lab testing were disproportionally affected by the crisis, with 72% suspending operations during the current COVID-19 pandemic.
- On the other hand, 79% of sleep centers that offer HSTs maintained some or all home testing volumes during the crisis.
 In 48% of those cases, respondents reported growth in immediate demand and/or additional technology investments to meet HST demand.
In 48% of those cases, respondents reported growth in immediate demand and/or additional technology investments to meet HST demand.- Sleep centers offering Telehealth consultation and appointment options (64%) now outnumber those that don’t offer those tech services (36%).

 In 48% of those cases, respondents reported growth in immediate demand and/or additional technology investments to meet HST demand.
In 48% of those cases, respondents reported growth in immediate demand and/or additional technology investments to meet HST demand.