Novel Narcolepsy Research Tops the 2022 FAST Conference Event Takeaways List
The 2022 Florida Association of Sleep Technologists (FAST) Conference featured an outstanding list of speakers and conversations. The one that stood out the most to the EnsoData team members in attendance was a presentation on novel narcolepsy research. The presentation touched on the two main types of narcolepsy, the differences in symptoms and challenges patients of the two types face, how a unique blood test can accurately expedite the diagnosis, and even how in-lab sleep testing may contain the information we need to more accurately diagnose narcolepsy types earlier in the process. The novel narcolepsy-related concepts were presented by Dr. Shane Drahos, the Chief of Sleep Medicine at Orlando VA Medical Center, who earned his sleep fellowship under Dr. Emmanuel Mignot at Stanford Medicine.Identifying and Treating Type 1 and Type 2 Narcolepsy
Narcolepsy is a sleep disorder that affects between 135,000 – 200,000 Americans. The primary symptoms for narcolepsy include excessive daytime sleepiness, poor REM sleep, loss of muscle tone, and sleep paralysis, among other challenges. However, symptoms differ between the two main types of narcolepsy, simply named Type 1 and Type 2. Generally speaking, Type 1 narcolepsy requires the patient to also suffer from cataplexy, while Type 2 does not. Per the National Institute of Neurological Disorders and Stroke, Type 1 patients not only present with excessive daytime sleepiness, but also present with cataplexy, and often are associated with a deficiency of hypocretin. Meanwhile, patients struggling with Type 2 narcolepsy still experience excessive daytime sleepiness, but usually have normal levels of hypocretin. In most Type 2 cases, patients have more subtle symptoms. And while some treatment options for Type 1 and Type 2 narcolepsy are similar, there are important differences when addressing cataplexy concerns. While there is no cure for narcolepsy, managing symptoms can make life more tolerable. To combat excessive daytime sleepiness, physicians often prescribe a central nervous system stimulant to help patients sleep at night. Conversely, amphetamine-like stimulants can be used during the day to help patients remain alert and focused. Unfortunately, for patients with cataplexy, an entirely different treatment is required. To treat cataplexy, physicians may prescribe a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI), a tricyclic antidepressant, or a central nervous system depressant.What does this mean for patients?
These medications alter the neurotransmitters used to communicate between brain cells to combat the patient’s cataplexy symptoms. It’s crucial to have these different medications working in tandem, as addressing excessive daytime sleepiness is only half the battle for Type 1 patients. Only receiving half the treatment isn’t likely to create successful long-term patient outcomes. And unfortunately, differentiating between the two types can often take years, as cataplexy doesn’t always present directly. The solution? Earlier diagnosis, via novel testing options.Blood Testing to Determine Narcolepsy Types
One of those novel testing options is the HLA-DQB1 blood test. Dr. Drahos highlighted how valuable it is in diagnosing which type of narcolepsy a patient has, noting that if the HLA-DQB1 test is negative, it is very unlikely for a patient to have Type 1 narcolepsy. How does this test work? This test is looking for an autoimmune factor and if it is positive, then it is likely a Type 1 diagnosis. Per Dr. Drahos, this simple fact indicates that Type 1 narcolepsy is an autoimmune disease and could also be triggered by certain illnesses, including H1N1, Strep throat, and possibly even the Coronavirus. As mentioned above, a patient can not be diagnosed as Type 1 unless there is a cataplexy component. However, Type 2 patients could potentially fail to display cataplexy for years after the initial diagnosis. That means they may not be able to receive the correct treatment up front.“This would mean that the person has always been Type 1, which is important for treatment purposes. Using the HLA-DQB1 test and also testing the levels of Hypocretin would lead to more accurate and timely diagnosis,” shared Jessica Moore, RPSGT, a 2022 FAST Conference attendee/vendor.Unfortunately, the test for hypocretin is a lumbar puncture which is painful and invasive, so it is not routinely done. Additionally, the HLA-DQB1 test is still “not readily used for diagnostic purposes,” meaning that not only do patients not have an accurate diagnosis up front, there are still challenges ahead for the novel blood testing research.
Can Sleep Tests Solve this Challenge?
Research published by Stephansen, J.B., Olesen, A.N., Olsen, M. et al (including Dr. Mignot) references both the HLA-DQB1 blood test and also the hypodensity graphs below which help identify stark differences between patients with narcolepsy and non-narcoleptic subjects. The research team leveraged a machine learning approach (neural networks) on a 3,000 patient dataset. The neural network approach allowed the team to automate sleep staging (down to 5s timeframes vs 30s epochs) and produce a hypodensity graph. A hypodensity graph is “a probability distribution conveying more information than classical hypnograms.” Below are two examples of hypodensity graphs from the Stephansen, et. al research.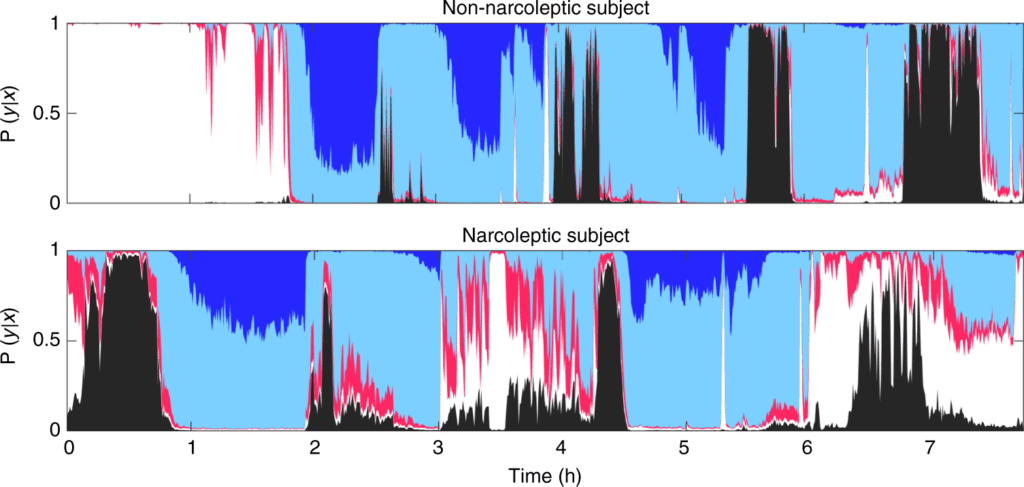
Data presented at the 2022 FAST Conference and originally published by Stephansen et. al. in 2018. Learn more: https://www.nature.com/articles/s41467-018-07229-3/figures/3
Moore added: “As a sleep technologist, I have observed multiple spontaneous arousals, REM bursts throughout all stages of sleep and a very high percentage of REM sleep in patients who ultimately received a narcolepsy diagnosis. Also, if you see a sleep onset REM period (within 15 minutes of beginning of test), there is a higher probability of narcolepsy, as well.”Dr Drahos also indicated that the reliability of the MSLT is valuable for Type 1 diagnosis, but does not provide a reliable result for Type 2. This paradigm was researched by Ruoff C, Pizza F, Trotti LM, et. al., with the result in the title: “The MSLT is Repeatable in Narcolepsy Type 1 But Not Narcolepsy Type 2: A Retrospective Patient Study.” However, when you combine all these novel approaches, you can paint a much clearer picture for each patient struggling with narcolepsy.