See how Total Sleep Time can improve confidence in results generated from your sleep clinic’s home sleep apnea testing (HSAT) program
If you’re reading this post, you likely have a few questions about EnsoSleep Total Sleep Time (TST) for sleep centers. TST can make a major difference in patient outcomes and experiences, and we’ll dive into how it does that in this post. We’ll also answer the following questions:
- What is the clinical value of measuring TST?
- How does EnsoSleep’s TST impact Patient AHI Severity Levels?
- Does TST work for all home sleep apnea testing (HSAT) devices?
- What does EnsoSleep’s TST cost?
With that laid out, let’s dive in.
What is the clinical value of Total Sleep Time?
While in-lab studies record signals that can be reviewed to determine whether the patient is asleep or awake (and what stage of sleep), not all home sleep studies include these signals. This makes it very difficult to determine how long a patient was asleep during their home sleep study.
Because of this, many home sleep apnea testing devices simply lean on the total recording time or total monitoring time instead.
Total recording time (TRT) and total monitoring time (MT), which do not account for the time it takes to fall asleep, any bathroom breaks, or other disturbances in the night, are often used by HSAT devices. Because these measurements do not take into account the times a patient is awake during the night, the “total sleep time” (TST) is artificially inflated.
However, adding an accurate total sleep time, like EnsoSleep TST, allows sleep labs to better assess the time a patient sleeps. EnsoSleep uses the signals already collected in HSAT devices to generate the sleep time, which in turn, leads to a more accurate calculation of the Apnea-Hypopnea Index (AHI).
You might be asking: “why is that important?” Let’s explain.
How does EnsoSleep’s TST impact Patient AHI Severity Levels?
When calculating the AHI of a patient, it’s commonly known that you take the number of sleep disordered breathing events (apneas and hypopneas) and divide by the denominator, which in the AHI equation is the time the patient slept. This is why it’s crucial to get the “time” component right.
Because obtaining an accurate AHI is so critical to identifying the best treatment plan, it’s crucial that the denominator accurately reflects the time the patient is asleep. A patient can easily change from an inconclusive or negative sleep apnea diagnosis to a mild sleep apnea diagnosis or jump to another sleep apnea severity level with even a minor change in the denominator.
Each sleep apnea severity level has a different treatment plan, and successful outcomes start with getting patients an accurate diagnosis and the best treatment option from the start. That’s why including an accurate TST in your HSAT analysis can allow physicians to identify the best treatment plan for each and every patient.
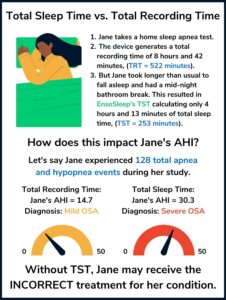
Let’s look at a specific, albeit extreme example outlined below, where Jane, a sleep patient taking an HSAT, shifts from a moderate OSA diagnosis to a severe OSA diagnosis based on the time differential that stemmed from a longer than usual amount of time to fall asleep (also known as sleep latency) and a middle of the night bathroom break.
As you can see, Jane didn’t sleep well during the night. Because she spent a lot of time tossing and turning while awake and wearing the device, the TRT measured 522 minutes. However, EnsoSleep TST calculated only 253 minutes, changing the denominator (or the “time” element) in the equation significantly enough to bump Jane up two full AHI sleep apnea severity levels.
This case may be extreme, but this same equation impacts all your HSAT patients. For example, another patient who might appear to have an AHI of just 4.5 might in fact be closer to 8, 9, or 10 when using TST instead of TRT or MT.
In short, by adding the power of total sleep time to your existing home sleep apnea testing devices, you can increase the chances of identifying the correct AHI severity level and getting each patient on the best possible treatment plan as a result.
Does EnsoSleep TST work for all home sleep apnea testing (HSAT) devices?
EnsoSleep total sleep time produces an accurate sleep time for most airflow-based HSAT devices. For specific information on devices, please reach out to our team by filling out the form on our Total Sleep Time page.
Because EnsoSleep is interoperable with all your devices, it allows sleep teams to standardize scoring results, leading to improved confidence among physicians. We are also continuing to add support for new devices and device types, so stay tuned for future updates. If you’d like to talk to an EnsoData team member about other device compatibilities that are coming in the future, schedule an EnsoSleep Demo or simply connect with someone on the team.
What does EnsoSleep’s TST cost?
There is no additional cost for EnsoSleep to calculate Total Sleep Time.
However, the value According to the 2022 Medicare Physician Fee Schedule, the 2022 average national reimbursement payment for sleep tests billed at 95800 is $66.54 more per test than 95806, and the only difference: 95800 tests must include “sleep time.”
Ultimately, when considering a base price of $10.75 per study and a possible reimbursement increase of $66.54 per test, we think this is the data point to help convince even the most frugal of financial managers.
As a disclaimer: We are not and cannot provide billing or reimbursement advice. Not every sleep test will qualify for the 95800 code, so we strongly advise you consult your Medicare contractor or payor organization with regard to local reimbursement policies. For more information, please refer to our HSAT Billing and Coding Guide.
EnsoSleep Total Sleep Time: The Solution your Organization Needs
Total Sleep Time is a win for your patients and your pocketbook. What are you waiting for? Schedule an EnsoSleep demo now.
TST – Request a Demo
"*" indicates required fields