Leverage Hypoxic Burden and other advanced metrics in EnsoSleep and EnsoSleep PPG Study Management to help illustrate the impact of sleep apnea on patients’ overall health
In sleep medicine, data tells the story. The more data you have, the more complete the story. And sometimes, you can look at the same raw data in a new way and discover new, advanced metrics. At EnsoData, we are constantly researching the best available clinical metrics to tell a more complete sleep story. These advanced metrics now include Hypoxic Burden information.
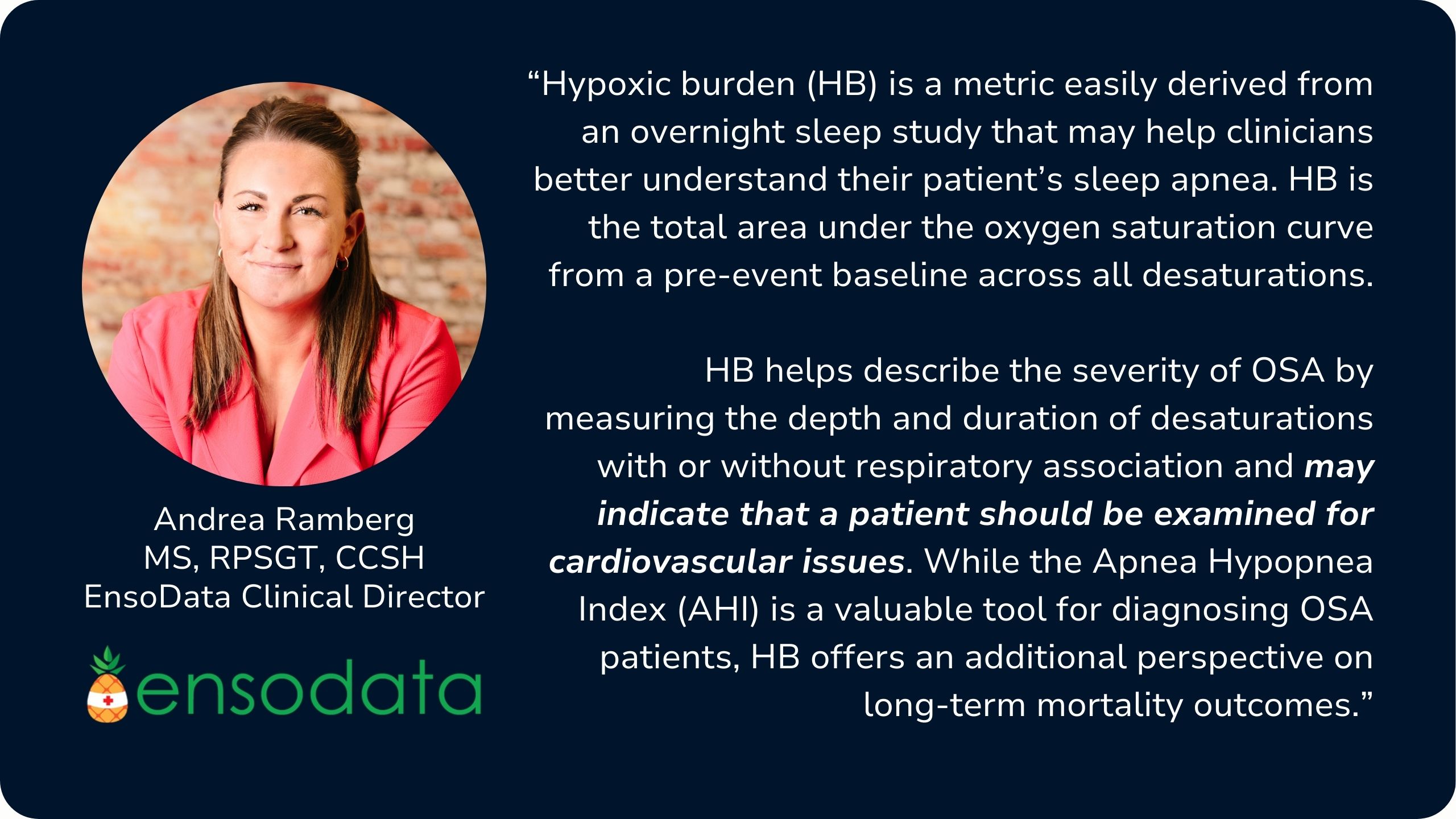
So, let’s examine hypoxic burden (HB), how to read HB data, how HB is displayed in EnsoSleep Study Management, how HB may serve as a predictor of cardiovascular and all-cause mortality, and how adding advanced metrics like HB may improve interpretation capabilities for sleep professionals.
How does Hypoxic Burden impact sleep study interpretation?
Hypoxic burden describes the severity of OSA by measuring the depth and duration of desaturations. The two most common existing AASM-recommended metrics used for describing this severity are the apnea-hypopnea index (AHI) and the oxygen desaturation index (ODI), but these metrics describe only the frequency of disordered breathing events and not their depth or duration.
Consider two similar patients, Fred and Greg. Both are males in their early 60s. Both have home sleep apnea studies showing an AHI of 33 and an ODI of 30. Relying on these two metrics alone, you might infer that sleep apnea affects each of them equally.
By adding hypoxic burden, we can see that Fred’s sleep apnea is causing far worse problems for his cardiopulmonary health. At each apnea, Fred typically desaturates 6-10% where Greg desaturates only 3%:
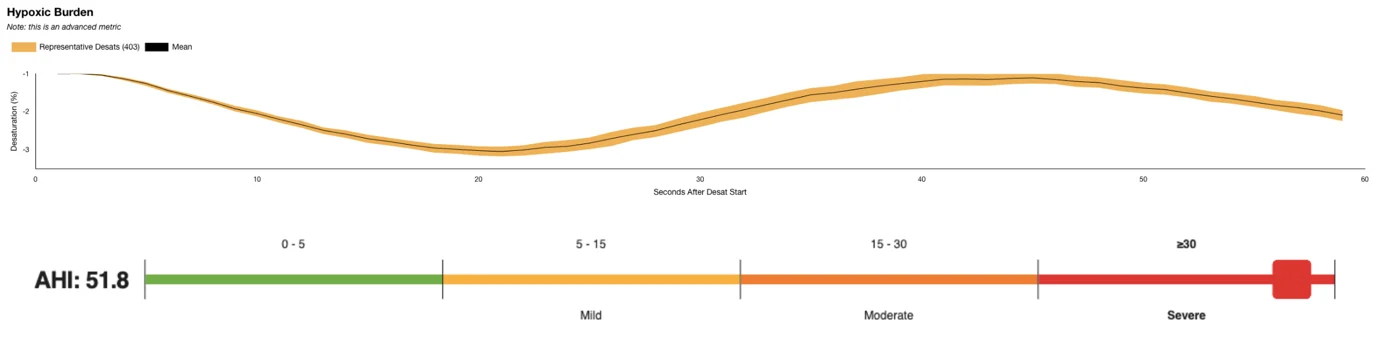
Hypoxic Burden charts in EnsoSleep Study Management stack all the desaturations in a study on top of each other. The dark mean line in the center shows, on average, to what depth and for what duration the patient experiences most desaturations. The yellow region around the mean line shows the trajectory of the 95th percentile of all the desaturations in the study.
Peer-reviewed, published literature (1) shows that longer and deeper desaturations were associated with the worsening of sleep apnea disease burden over a 5-year period and that “incorporating the duration and depth of respiratory events and their associated desaturations could provide useful information in identifying and managing OSA patients with greater precision.”
While hypoxic burden is still too new to be recommended by the AASM, it is a valuable data point for clinical decision making. HB is defined as the total area above the oxygen saturation curve during a desaturation.
How to Read Hypoxic Burden Data
For each desaturation, the metric is calculated by counting at each percentage point downward step in the oxygen saturation and multiplying by the fraction of minutes that desaturation is sustained. This number is reported as percent times minutes, (% min). Like other sleep indexes, the total amount of % min is added up across all desaturations and then divided by the total hours of sleep time, resulting in the strange unit of % min / hr.
So in other words, the larger the area above the saturation curve, the more time and greater the depth of desaturations and the higher the hypoxic burden.
Hypoxic Burden Severity in an Age- and Gender-Aware Context
We recognize that hypoxic burden and its numeric output such as “68.8 %-min/hr” is not yet widely understood in the sleep provider community. EnsoData’s hypoxic burden data is collected and validated on a patient cohort of 201,116 historical sleep studies.
“The total hypoxic burden for the patient was 68.84 % min / hr based on 403 desaturation events. We recommend…”
You have the choice to report a more in-depth summary in an age- and gender-aware matched cohort from a smaller subset of studies, that correspond to the specific gender and age cohort matching a given sleep study. For example:
“The 3% hypoxic burden value calculated for this study is 68.84 % minutes per hour. This is based on the 403 desaturation events you experienced through the night divided by your total sleep time. Your HB is more severe than 73% of men aged 60-70 in an age- and sex-matched clinical cohort of more than 11,000 patients, (0 is least severe, 100 is most severe). Insert clinician/physician recommendations here.”
By leveraging the HB chart and recommendations in Study Management, you can highlight the critical importance of treating sleep apnea, as HB serves as a potential predictor of long-term cardiovascular risk. This empowers you to take a more persuasive and proactive approach, encouraging patients to pursue essential treatment and referrals to specialist care that can save lives.
Per Andrea Ramberg, MS, RPSGT, CCSH, and EnsoData Clinical Director, this new information is set to add an important perspective on long-term health outcomes.
Hypoxic Burden shows promise in predicting cardiovascular and all-cause mortality
Advanced HB data not only allows you to more deeply understand the severity of a patient’s OSA, but also what might be ailing patients beyond OSA, as HB helps uncover other comorbid health issues.
Across specialties, hypoxic burden information may be a potential predictor of a number of negative cardiovascular outcomes, including heart failure (2), cardiovascular mortality (3), stroke (4), blood pressure changes (5), and other negative outcomes, like kidney disease (6).
In 2019, Azarbarzin and colleagues demonstrated that HB predicted cardiovascular mortality and all-cause mortality much better than either AHI or ODI in a study of thousands of patients. For a more detailed explanation, please reference the full 2022 Martinez-Garcia, et. al. study.
For a deeper understanding of the clinical relevance of hypoxic burden and the long-term implications a high HB can have on patients, we recommend diving into the literature linked in the article. And if you’re an EnsoData customer and would like to add HB to your reports, please contact your EnsoData CSE at support@ensodata.com.
References:
- Martinez-Garcia, et. al: https://pubmed.ncbi.nlm.nih.gov/36115739/
- Azarbarzin, A, et. al: https://pubmed.ncbi.nlm.nih.gov/32298733/
- Butler, M, et. al: https://pubmed.ncbi.nlm.nih.gov/30336691/
- Blanchard, M, et. al: https://pubmed.ncbi.nlm.nih.gov/33214210/
- Kim JS, et. al: https://pubmed.ncbi.nlm.nih.gov/31439722/
- Jackson, C, et. al: https://pubmed.ncbi.nlm.nih.gov/33277428/






