Did the SLEEP 2021 virtual conference change the way you are thinking about patient care in sleep medicine?
Note: Presentations and content will only be available for people who registered for SLEEP 2021 until November 30th, 2021. What a conference! SLEEP 2021 certainly did not let us down, as the APSS (Associated Professional Sleep Societies) team really brought its “A” game. Where to start? It is easy to jump to the opening plenary session, which spawned a lot of questions about the future of sleep medicine and insomnia. The research presented by Dr. Eus JW Van Someren set the stage for the rest of the conference: change is inevitable. There were several key themes from the SLEEP 2021 conference, but one stood out above the rest: data is the future. Physicians and researchers alike are recognizing the power in the data: from improving compliance rates to studying for better biomarkers indicating nuanced comorbidities. We’re completely onboard the data train, and believe optimized applications of data are the future of sleep medicine. Let’s jump into some of our favorites, and a few of the SLEEP 2021 takeaways from the virtual event.Artificial Intelligence and Sleep in the 21st Century and Beyond
The first session we’re highlighting is from the tech track. In his presentation, Dr. David Kent tackled the subject we hold near and dear: AI and Sleep Medicine. There is a trend in sleep of shifting from being diagnostically-focused to more outcome-focused, specifically getting patients treated quickly and improving adherence rates. Dr. Kent discussed how this focus on the human component can be further supported by AI, and he demonstrated how ML and AI have the potential to change sleep medicine in 3 ways by:- Making routine processes more efficient. In this example, he highlighted how automated PSG scoring can free up sleep techs for more proactive, complex tasks, from remote monitoring to patient education.
- Improving access. In this example, Dr. Kent proposes a higher clinical lab throughput based on better automation, as staff are freed up to help improve efficiency.
- Expediting the discovery of new clinical data patterns. In this final example, he highlighted the novel associations between the PSG data, demographics, and genetic data that will improve disease diagnosis and treatment, in other words: “phenotype discovery.”
- Be incorporated into existing clinical workflows, from automated PSG staging and scoring to automated PAP monitoring with alerts,
- Drive the development of novel workflows for existing pathology, from consumer wearables for common disease screening,
- Expedite the discovery of disease endotypes that will result in new management and treatment pathways.
Habitual Sleep Duration and Chronic Pain in the US Population Over A 10-Year Period: Implications for Sleep Health Disparities
Everyone has a loved one who suffers from arthritis, joint pain, back pain, and other types of chronic pain. This chronic pain is a significant impairment to one’s daily life, and an individual’s sleep habits may be able to help improve quality of life and reduce this chronic pain. In this session, Chloe Craig shared the University of Arizona research on the relationship between pain and sleep. That relationship is a 2-way street. Chronic pain impairs sleep, and poor sleep can worsen pain experiences. In their research, Craig, et. al. sought to answer two primary questions. First, is habitual sleep duration associated with specific chronic pain conditions? And second, does the relationship between sleep duration and chronic pain conditions depend on race/ethnicity? Dive into all the answers by watching on-demand, but for a sneak peek, here’s one of the deck’s most interesting graphs: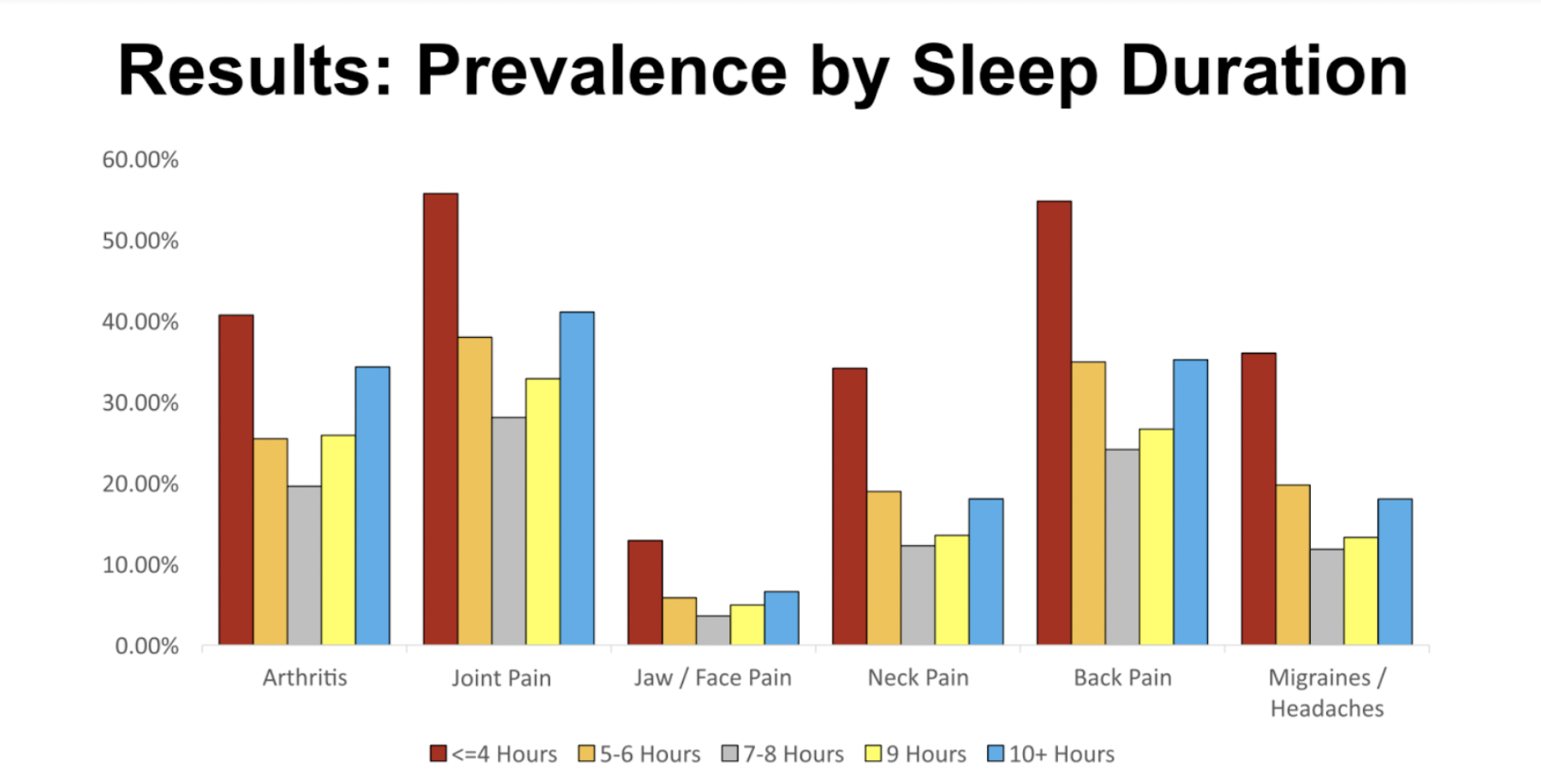 As you can see, there is significantly increased pain across the board for people who sleep less than 4 hours, and in all cases, getting 7-8 hours of sleep leads to the least amount of pain.
Per Craig, the COVID-19 pandemic highlighted the disproportionate health effects that minority groups experience. Not displayed here, but outlined in the deck, Craig emphasized a number of eye opening statistics relating to minority groups. Chief among them being that minority groups who get less than 7 hours of sleep per night are more likely to develop obesity, hypertension, and diabetes than other groups with similar sleep patterns. At the end of the day, sleep is another area of disparity for minority populations.
As you can see, there is significantly increased pain across the board for people who sleep less than 4 hours, and in all cases, getting 7-8 hours of sleep leads to the least amount of pain.
Per Craig, the COVID-19 pandemic highlighted the disproportionate health effects that minority groups experience. Not displayed here, but outlined in the deck, Craig emphasized a number of eye opening statistics relating to minority groups. Chief among them being that minority groups who get less than 7 hours of sleep per night are more likely to develop obesity, hypertension, and diabetes than other groups with similar sleep patterns. At the end of the day, sleep is another area of disparity for minority populations.
From Crime to COVID: Disparities in Sleep and What We Can Do About It
In this session, we hear from Wendy Troxel, PhD, on the impact of race on sleep health. Systemic racism disproportionately exposes minorities to income inequities, redlining, urban renewal, forced relocation, and police brutality, all of which are directly linked to sleep health, highlighted Troxel. Food insecurity disproportionately affects minority households. Additionally, minorities are associated with detrimental health outcomes like obesity risks and cardiometabolic disease. There has also been relatively little research on the correlation between food insecurity and sleep health. So, what can you do? Troxel recommends:- Holding gatherings for the community to discuss wellness topics and educate on sleep health interventions,
- Performing outreach work with the community and politicians,
- Trying to better understand the lived experience.
Sleep to Change Your Mind
In the final presentation we’ll highlight, we learned from Dr. Gina R Poe of the UCLA Integrative Biology and Physiology department. Dr. Poe was one of the more entertaining and digestible sessions of the Friday sessions. Among topics, Dr. Poe covers the importance of REM sleep. She especially dove into the lifecycle of REM sleep for humans, starting with infancy when REM is absolutely crucial, paraphrased here: “When we learn things – when we form new words or learn to walk – we’re also pruning away the features that are not normal / consistent. That pruning activity is super important during early development, and REM is so important to that learning and pruning to set up our world schema.” When it comes down to it, schemas about the world are highly relevant to mental health and developmental processes, and limiting the development of those schemas (due to poor sleep) can be a longer-term issue.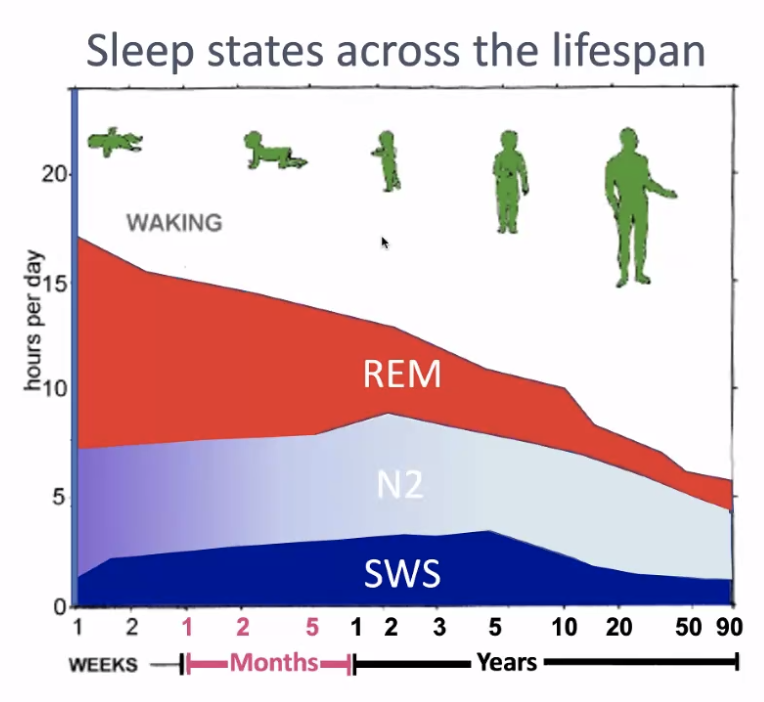
As you can see, for infants under one, the REM cycles are far more prevalent, allowing for more nuanced development.